Fungal : 45 year old female
date of admission 8/5/2024
date of discharge 12/5/2024
ACUTE ON CHRONIC RESPIRATORY FAILURE WITH HYPOXIA SECONDARY TO LOWER RESPIRATORY TRACT INFECTION (COMMUNITY AQUIRED PNEUMONIA)
-CAVITATION IN LEFT APEX ? FUNGAL BALL CHRONIC ASPERGILLOSIS
-CORPULMONALE
-TRACTION BRONCHIECTASIS OF BOTH LUNGS
-H/O PULMONARY KOCHS 15 YEARS AGO
-K/C/O DM SINCE 10 YEARS HYPERTENSION SINCE 5 YEARS
Case History and Clinical Findings
PATIENT COMPLAINS OF SHORTNESS OF BREATH SINCE 6 DAYS
HOPI:-PATIENT WAS APPRENTLY ASYMPTOMATIC 6 DAYS AGO THEN SHE DEVELOPED SHORTNESS OF BREATH GRADE-III NYHA WHICH GRADUALLY PROGRESSED TO GRADE-IV NYHA SINCE 2 DAYS INSIDIOUS IN ONSET.
H/O 2 EPISODES OF VOMITING,GREENISH IN COLOUR,CONTAINED FOOD PARTICLES SINCE TODAY MORNING.
H/O COUGH +2-3 EPISODES NON PRODUCTIVE TYPE INITIALLY NOT ASSOCIATED WITH POST TUSSIVE VOMITING, LATER PRODUCTIVE WITH YELLOW SPUTUM.
NO H/O ,LOSS OF CONSCIOUSNESS,LOOSE STOOLS,CONSTIPATION,BURNINGMICTURITION,CHEST PAIN,PALPITATION.
H/O FEVER 1 DAY BACK FOR 3 DAYS HIGH GRADE, INTERMITTENT TYPE, RELIEVED ON MEDICATION
NO H/O HEMOPTYSIS, WEIGHT LOSS, LOSS OF APPETITE
H/O SIMILAR COMPLAINTS 15 YEARS AGO AND 8 MONTHS AGO FOR WHICH SHE WAS ADMITTED AND TREATED WITH ATT, INTERMITTENT CPAP, O2 SUPPORT, BRONCHODILATORS AND MUCOLYTICS.
K/C/O PULMONARY TUBERCULOSIS 15 YEARS BACK TOOK ATT FOR 6 MONTHS
K/C/O TYPE-2 DIABETES MELLITUS SINCE 10 YEARS ON T.SITAGLUIPTIN 50 MG + T.METFORMIN 500MG
K/C/O HYPERTENSION SINCE 6 YEARS ON T.AMLO-AT 5/50MG
PERSONAL HISTORY:-
APETITE-NORMAL
BOWEL AND BLADDER-REGULAR
ALLERGIES-NIL
ADDICTIONS-NIL
FAMILY HISTORY:-NOT SIGNIFICANT
GENERAL EXAMINATION:-
PATIENT IS CONSCIOUS,COHERENT,CO-OPERATIVE
NO SIGNS OF PALLOR,ICTERUS,CYANOSIS,CLUBBING,LYMPHADENOPATHY.
BILATERAL PEDAL EDEMA +, PITTING EDEMA
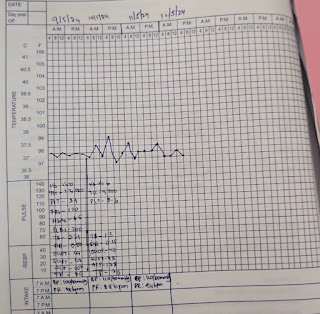
VITALS AT ADMISSION :
BP-150/100 MMHG
TEMP:-98.6
PR:-84BPM
RR:-24CPM
SPO2 - 56% @ RA
GRBS:-260MG/DL
SYSTEMIC EXAMINATION:-
CVS:-S1 S2 HEARD NO MURMURS
RS:- BILATERAL AIR ENTRY+; EXPIRATORY WHEEZE+ IN RIGHT MAMMARY, INFRACLAVICULAR, LEFT MAMMARY AREA; CREPITATIONS + IN B/L BASAL AREAS (MA, IAA, ISA)
PER ABDOMEN:-NO TENDERNESS
NO ORGANOMEGALY
CNS:-NO FOCAL NEUROLOGICAL DEFICITS NOTED
COURSE IN THE HOSPITAL
A 45 YEAR OLD FEMALE PATIENT, WHO IS A KNOWN DIABETIC, HYPERTENSIVE AND WITH HISTORY OF PULMONARY TUBERCULOSIS (15YRS AGO) WAS BROUGHT TO CAUALTY WITH C/O SHORTNESS OF BREATH SINCE 6 DAYS, GRADE III NYHA, EXACERBATED SINCE 2DAYS TO GRADE IV NYHA. THOROUGH CLINICAL EVALUATION WAS DONE AND NECESSARY INVESTIGATIONS WERE SENT.
CPAP SUPPORT WAS INITIATED, O2 SUPPLEMENTATION WAS GIVEN AND CONSERVATIVE MANGEMENT WAS STARTED.
AFTER TAKING BLOOD, URINE AND SPUTUM CULTURES WERE SENT AND IV ANTIBIOTICS WERE STARTED.
2DECHO WAS DONE WHICH SHOWED [(ECCENTRIC TR+) MODERATE TR+ WITH MILD PAH;TRIVIAL AR+, NO RWMA.NO AS/MS.NO MR ,EJECTION FRACTION=68%;RVSP-51MMHG, GOOD LV SYSTOLIC DYSFUNCTION, GRADE-I DIASTOLIC DYSFUNCTION, NO LV CLOT] &USG ABDOMEN WAS DONE WHICH SHOWED CHOLELITHIASIS(12MM), LEFT MILD PLEURAL EFFUSION, RIGHT GRADE 1 RPD CHANGES.
OUTSIDE CT SCAN SHOWED LEFT MODERATE AND RIGTH MILD PLEURAL EFFUSION, DEPTH MEASURING 3CVM AND 8CM ON LEFT &RUGHT RESPECTIVELY, CAVITATION IN LEFT APEX WITH DEPENDENT SOLID COMPONENT, PROBABLE FUNGAL BALL, E/O CYSTIC AND TRACTION BRONCHECTATIC CHANGES WITH FIBROSTREAKY OPACITIES IN BOTH LUNGS, LOSS OF LUNG VOLUME ON RIGHT SIDE.
PATIENT IS PROVISIONALLY DIAGNOSED WITH REACTIVATION OF TUBERCULOSIS/LRTI (?COMMUNITY ACQUIRED PNEUMONIA)
PULMONOLOGY OPINION WAS TAKEN FOR BRONCHOSCOPY AND BRONCHOALVEOLAR LAVAGE. BUT THE PATIENT AND HER ATTENDERS WERE NOT WILLING FOR THE SAID PROCEDURE AND REFUSED TO GIVE CONSENT AND WANT TO GET IT DONE ON FOLLOW UP.
DURING THE COURSE IN THE HOSPITAL, PATIENT HAD NO FEVER SPIKES, SHORTNESS OF BREATH REDUCED, O2 REQUREMENT REDUCED.
DURING THE COURSE OF STAY PATIENT WAS TREATED WITH IV ANTIBIOTICS, ANIFUNGALS, PPIS,ANTIPYRETICS, CORTICOSTEROIDS, DIURETICS, MUCOLYTICS, BRONCHODILATORS, EXPECTORANTS, OHAs AND OTHER SUPPORTIVE DRUGS.
DURING THE COURSE OF STAY IN THE HOSPITAL, PATIENT IMPROVED IN CONDITION. HENCE THE PATIENT IS BEING DISCHARGED IN HEMODYNAMICALLY STABLE CONDITION WITH HOME OXYGEN SUPPORT (@2-4 LIT TO MAINTAIN SPO2 >92%)
Investigation
HBsAg-RAPID 09-05-2024 01:01:AM Negative
Anti HCV Antibodies - RAPID 09-05-2024 01:01:AM Non Reactive
HIV 1/2 RAPID:-NEGATIVE
BGT:- A POSITIVE
ABG 08-05-2024 09:39:PMPH 7.371PH 7.371PCO2 41.4PCO2 41.4PO2 46.1PO2 46.1HCO3 23.4HCO3 23.4St.HCO3 22.6St.HCO3 22.6BEB -1.3BEB -1.3BEecf -1.1BEecf -1.1TCO2 44.8TCO2 44.8O2 Sat 73.9O2 Sat 73.9O2 Count 17.9O2 Count 17.9
RBS ON 9/5/24 :-262 MG/DL
BLOOD UREA 09-05-2024 :-23 mg/dl
SERUM ELECTROLYTES (Na, K, C l) 09-05-2024 01:00:AMSODIUM 138 mmol/LPOTASSIUM 3.9 mmol/L CHLORIDE 101 mmol/L
SERUM CREATININE 09-05-2024 01:00:AM :-1.0 mg/dl
LIVER FUNCTION TEST (LFT) 09-05-2024 01:00:AMTotal Bilurubin 2.39 mg/dl Direct Bilurubin 0.60 mg/dl SGOT(AST) 44 IU/L SGPT(ALT) 49 IU/LALKALINE PHOSPHATASE 207 IU/L TOTAL PROTEINS 8.9 gm/dl ALBUMIN 4.52 gm/dl A/G RATIO 1.03
BLEEDING TIME:-3 MIN
CLOTTING TIME:-4 MIN 30 SEC
APTT:-35 SEC
PT:-17
INR:-1.25
COMPLETE URINE EXAMINATION (CUE) 09-05-2024 01:00:AMCOLOUR Pale yellowAPPEARANCE ClearREACTION AcidicSP.GRAVITY 1.010ALBUMIN TraceSUGAR NilBILE SALTS NilBILE PIGMENTS NilPUS CELLS 2-4EPITHELIAL CELLS 2-3RED BLOOD CELLS NilCRYSTALS NilCASTS NilAMORPHOUS DEPOSITS AbsentOTHERS Nil
HEMOGRAM:-(9/5/24)
HB:-14 GM/DL
TLC:-12,500 CELLS/CUMM
PCV:-44.3%
MCV:-87.6 FL
MCH:-29.3 PG
MCHC:-33.4%
RBC:-5.0 MILLION/CU MM
PLATELET COUNT:-2.9 LAKHS/CU MM
IMPRESSION:-NCNC WITH LEUCOCYTOSIS
FBS:-120 MG/DL
HBA1C:-6.8%
PLBS:-200MG/DL
HEMOGRAM:-(10/5/24)
HB:-14.6 GM/DL
TLC:-9200 CELLS/CUMM
PCV:-42.6%
MCV:-87.9 FL
MCH:-30.1 PG
MCHC:-34.2%
RBC:-4.85 MILLION/CU MM
PLATELET COUNT:-2.6 LAKHS/CU MM
LIVER FUNCTION TEST (LFT) 10-05-2024
Total Bilurubin 1.30 mg/dlDirect Bilurubin 0.35 mg/dlSGOT(AST) 42 IU/LSGPT(ALT) 48 IU/LALKALINE PHOSPHATASE 178 IU/LTOTAL PROTEINS 7.6 gm/dlALBUMIN 3.8 gm/dlA/G RATIO 1.04
2D ECHO DONE ON 9/5/24:-
-(ECCENTRIC TR+) MODERATE TR+ WITH MILD PAH;TRIVIAL AR+
-NO RWMA.NO AS/MS.NO MR
-EJECTION FRACTION=68%;RVSP-51MMHG
-GOOD LV SYSTOLIC DYSFUNCTION
-GRADE-I DIASTOLIC DYSFUNCTION
-NO LV CLOT
-IVC SIZE(1.50CMS) COLLAPSING
-SCLEROTIC AV
-NO AS/MS
USG ABDOMEN WAS DONE ON 09/05/24
(SUBOPTIMAL SCAN)
IMPRESSION :
CHOLELITHIASIS (12MM HYPERECHOIC FOCUS)
LEFT MILD PLEURAL EFFUSION
RIGHT GRADE 1 RPD CHANGES
CT SCAN (OUTSIDE)
LEFT MODERATE AND RIGTH MILD PLEURAL EFFUSION, DEPTH MEASURING 3CVM AND 8CM ON LEFT &RUGHT RESPECTIVELY.
CAVITATION IN LEFT APEX WITH DEPENDENT SOLID COMPONENT, PROBABLE FUNGAL BALL
E/O CYSTIC AND TRACTION BRONCHECTATIC CHANGES WITH FIBROSTREAKY OPACITIES IN BOTH LUNGS.
LOSS OF LUNG VOLUME ON RIGHT SIDE
Treatment Given(Enter only Generic Name)
INJ.LASIX 40MG IV/TID X 5 DAYS
INJ.AUGMENTIN 1.2 GM/IV/BD X 5DAYS
INJ.PAN 40MG IV/OD
INJ.NEOMOL 1GM/IV/SOS
INJ.HYDROCORTISONE 100MG IV/SOS
INJ.HAI/SC/TID
T.AZITHROMYCIN 500 MG PO/OD X 4DAYS
T.ITRACONAZOLE 200MG PO/BD X 5DAYS
T.PULMOCLEAR PO/BD X 2DAYS
T.SITAGLIPTIN 50MG + T.METFORMIN 500MG PO/OD
SYP.ASCORIL-LS 10ML/PO/TID
NEB WITH DUOLIN 6TH HRLY
BUDECORT 8TH HRLY
MUCOMIST 6TH HRLY
INTERMITTENT CPAP
Advice at Discharge
HOME OXYGEN
TAB AUGMENTIN 625MG PO/BD FOR 2 DAYS 8AM AND 8 PM
TAB ITRACONOZOLE 200 MG BD AT 8 AM AND 8PM FOR 10 DAYS
TAB.DYTOR PLUS 10/50MG /PO/OD AT 8 AM TO CONTINUE
TAB TELMA 20MG/PO/OD AT 8 AM TO CONTINUE
TAB PAN 40MG PO/OD X 1 WEEK BEFORE BREAKFAST
T.AZITHROMYCIN 500 MG PO/OD AT 2PM X 1 DAY
T.PULMOCLEAR PO/BD AT 8 AM AND 8 PM X 5 DAYS
T.SITAGLIPTIN 50MG + T.METFORMIN 500MG PO/OD BEFORE BREAKFAST TO CONTINUE
TAB REJUNEX CD3 PO/OD AT 2 PM X 15DAYS
SYP.ASCORIL-LS 10ML/PO/TID AT 8 AM ,2PM AND 8 PMX 1 WEEK
NEB WITH DUOLIN 12TH HRLY
BUDECORT 12TH HRLY
MUCOMIST 12TH HRLY
HOME O2 SUPPORT @ 2-4 LIT TO MAINTAIN SPO2 >92%

Comments
Post a Comment